THE BEST NURSING CONCEPTS FOR CLINICAL JUDGMENT & THE NEW NCLEX
CLINICAL JUDGMENT: THE TOP 6 PRIORITY-SETTING FRAMEWORKS FOR THE NEW NCLEX (NEXT GEN NCLEX)
Strengthening students' clinical judgment skills is a fundamental aspect of preparing them for the NCLEX (now commonly referred to as the Next Generation NCLEX [NGN]). A nursing concept directly related to the development of clinical decision-making and judgment is priority setting.
Stay up-to-date on the NCLEX & Next Generation NCLEX.

Priority setting has become more important over the last couple of decades as healthcare has evolved. Patty Knecht, PhD, RN, ANEF, Vice President, Chief Nursing Officer at ATI and Ascend Learning, explains. “Nurses today have a much higher level of demand on their services,” she says. “That demand means they must ration the care they give. In other words, they must determine the priority of care that clients require as conditions change and needs arise.”
If the term priority setting doesn’t sound familiar, don’t worry. You’ve been teaching the technique, even if you haven’t been using that verbiage. Basically, priority setting is when you look at nursing problems in terms of urgency and/or importance to determine which ones to deal with first.
CLINICAL JUDGMENT & YOUR CHOICE OF PRIORITY FRAMEWORKS FOR THE NCLEX (AKA THE NEXT GEN NCLEX)
Before the Next Generation NCLEX launched, many nurse educators began reviewing their lesson plans and curriculum to determine which framework — or process — would be the best to use. (Some had mistakenly thought the National Council of State Boards of Nursing wanted educators to change which nursing framework they used. Retired Vice President and Chief Nursing Officer Dr. Sheryl Sommer explained why this wasn’t the case and how similar the most prominent frameworks were to one another in an article she wrote for Nurse Educator journal.)
You have a variety of priority-setting frameworks from which to choose in teaching your students, and chances are you’ve already been using one — or several — of them in your lessons. (Scroll down for details on the most common ones.)
DOWNLOAD THE INFOGRAPHIC AT RIGHT AS A HANDY REFERENCE
Why is it important to teach students about these frameworks? Doing so helps them learn to order their thinking and, therefore, advance their clinical judgment. Admittedly, students and new nurses probably can't immediately identify which framework they use as they assess client priorities. But, in time, these frameworks become an inherent part of their processing, and they automatically pick and choose among them to use the cognitive functions that best match the situation.
PREPARING FOR NCLEX WITH THE 6 MOST-COMMON PRIORITY-SETTING FRAMEWORKS FOR CLINICAL JUDGMENT
To help you in teaching these frameworks — in general and in preparation for the NCLEX (the Next Gen NCLEX) — we’ve broken out the 6 most common. We describe how the process works within each, then provide an item example and rationales for each answer. (We identify the correct answer and matching rationale in red.) Feel free to use these samples in your lessons.
The priority-setting frameworks described here are:
- Maslow’s Hierarchy of Needs
- The Nursing Process
- Airway – Breathing – Circulation
- Safety & Risk Reduction
- Least Restrictive/Least Invasive
- Acute vs. Chronic/Unstable vs. Stable/Urgent vs. Nonurgent.
PUTTING NURSING FRAMEWORKS INTO ACTION WITH STRATEGIES FOR NCLEX PREP
As you review each of these frameworks, consider the following strategies to help students improve their skills in prioritizing care:
- Use priority-setting NCLEX items as tools in the classroom or clinical post conference.
- Assign screen-based simulations or videos with clinical scenarios that require students to respond based on a particular priority-setting framework.
- Use priority-setting frameworks in classroom activities, such as case studies.
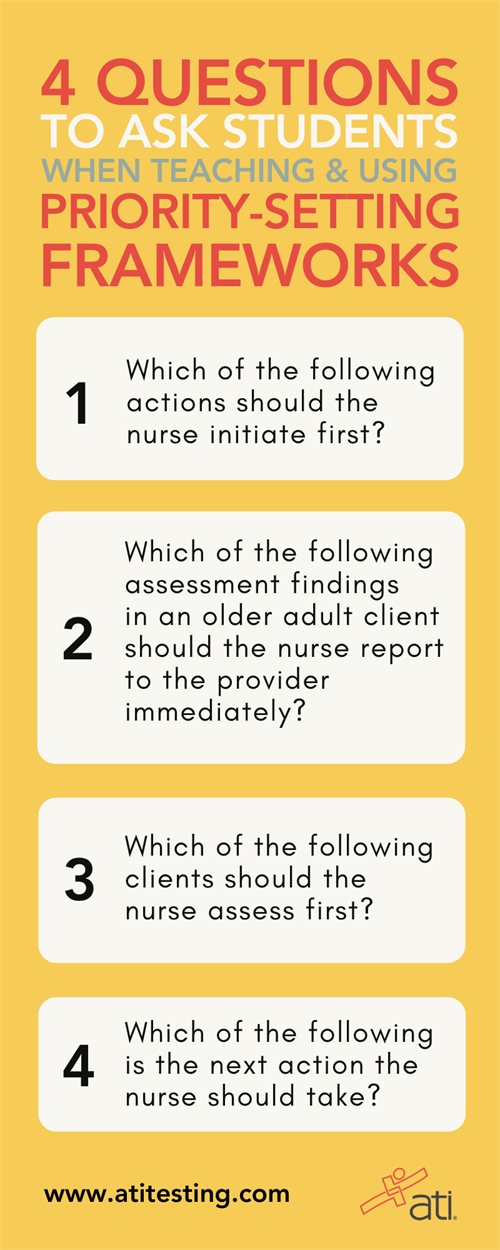
Some priority-setting questions you can use are:
- Which of the following actions should the nurse initiate first?
- Which of the following assessment findings in an older adult client should the nurse report to the provider immediately?
- Which of the following clients should the nurse assess first?
- Which of the following is the next action the nurse should take?
MASLOW'S HIERARCHY OF NEEDS: OPTION 1 FOR TEACHING CLINICAL JUDGMENT
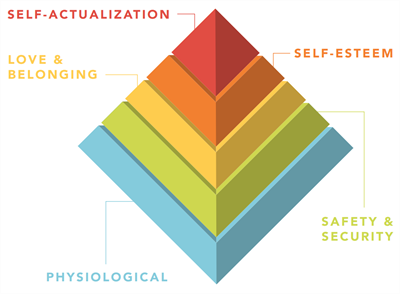 This framework contains 5 levels of prioritized needs. (See diagram at right.) Physiological needs supersede the others in most circumstances. However, all client factors should be considered before determining need order.
This framework contains 5 levels of prioritized needs. (See diagram at right.) Physiological needs supersede the others in most circumstances. However, all client factors should be considered before determining need order.
ITEM EXAMPLE
A nurse is planning care for a client who has bipolar disorder and is experiencing an acute manic episode. Which of the following is the highest priority intervention the nurse should include in the plan of care?
A. Give the client simple directions for completing ADLs.
B. Offer the client high-calorie fluids frequently.
C. Provide the client with structured solitary activities.
D. Keep the client’s valuables in a locked area.
RATIONALES
A. Clients who are having an acute manic episode are likely to have poor concentration and difficulty completing routine tasks. Providing simple directions for completing ADLs helps the client focus; however, it’s not the highest priority.
B. The priority action for a client who is experiencing an acute manic episode is to meet the client’s physiological need for food and water. Therefore, the priority intervention is to offer the client high-calorie fluids frequently to prevent calorie deprivation and dehydration.
C. Clients who are having an acute manic episode are likely to have difficulty focusing on any one activity. Providing the client with structured solitary activities helps provide focus and feelings of security; however, it’s not the highest priority.
D. Clients who are having an acute manic episode are likely to give away their valuables. Keeping the client’s valuables in a locked area prevents the client from doing so; however, it’s not the highest priority.
AIRWAY – BREATHING – CIRCULATION: OPTION 2 FOR TEACHING CLINICAL JUDGMENT
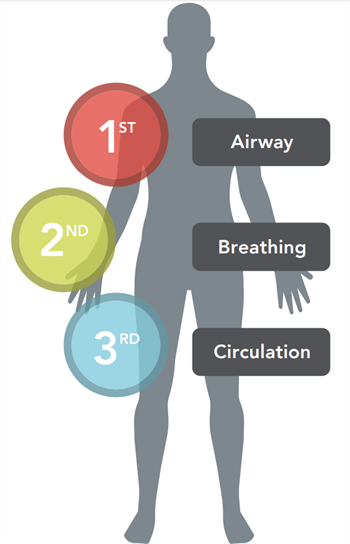 Often called the ABCs, this framework is always the priority for initial assessments when the client's life is at stake as all 3 attributes are essential for survival.
Often called the ABCs, this framework is always the priority for initial assessments when the client's life is at stake as all 3 attributes are essential for survival.
ITEM EXAMPLE
A nurse is caring for a client who is wheezing and gasping for breath just after receiving a dose of amoxicillin. Which of the following actions is the nurse’s priority?
A. Administer epinephrine parentally.
B. Provide reassurance to the client.
C. Initiate an IV infusion of 0.9% sodium chloride.
D. Place client on a cardiac monitor.
RATIONALES
A. The nurse’s priority is to give the client an injection of epinephrine, which will counteract the bronchoconstriction.
B. The nurse should reduce the client’s anxiety by providing reassurance; however, it’s not the nurse’s highest priority.
C. Starting an IV infusion of 0.9% sodium chloride is important to maintain fluid balance and provide venous access; however, it’s not the nurse’s highest priority.
D. Attaching the client to a cardiac monitor is important, because medications used to treat anaphylaxis can cause tachycardia and dysrhythmias; however, it’s not the nurse’s highest priority.
SAFETY & RISK REDUCTION: OPTION 3 FOR TEACHING CLINICAL JUDGMENT
 This framework establishes priority based on which situation poses the greatest threat to the client at that time. When multiple risks are present, another priority-setting framework, like the ABCs, may need to be used to identify the highest priority.
This framework establishes priority based on which situation poses the greatest threat to the client at that time. When multiple risks are present, another priority-setting framework, like the ABCs, may need to be used to identify the highest priority.
ITEM EXAMPLE
A nurse is planning care for a client who is in acute alcohol withdrawal. Which of the following medications should the nurse plan to administer first?
A. Disulfuram
B. Lorazepam
C. Clonidine
D. Atenolol.
RATIONALES
A. Disulfuram is given to support abstinence from alcohol and prevent relapse; however, this is not the greatest risk to the client at this time.
B. The greatest risk to the client during acute alcohol withdrawal is seizures. Therefore, the nurse should first administer lorazepam to control or minimize seizures.
C. Clonidine can help minimize the autonomic symptoms that occur with acute alcohol withdrawal; however, these are not the greatest risks to the client at this time.
D. Atenolol can help minimize the autonomic symptoms that occur with acute alcohol withdrawal; however, these are not the greatest risks to the client at this time.
THE NURSING PROCESS: OPTION 4 FOR TEACHING CLINICAL JUDGMENT
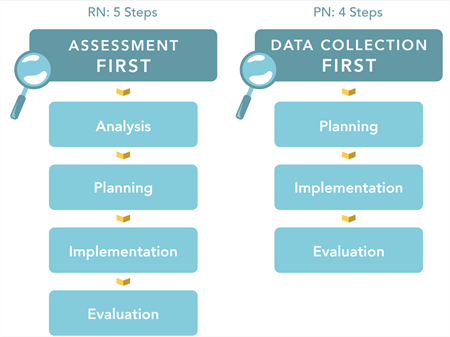 This framework — one of the most common in nursing programs — is a 4- or 5-step process (differing between RNs and PNs) that nurses use for decision-making. It helps determine priority nursing actions based on the steps in the diagram at right and always starts with assessment/data collection.
This framework — one of the most common in nursing programs — is a 4- or 5-step process (differing between RNs and PNs) that nurses use for decision-making. It helps determine priority nursing actions based on the steps in the diagram at right and always starts with assessment/data collection.
ITEM EXAMPLE
A nurse is caring for an adolescent who is to undergo an open reduction and internal fixation of the ankle following a sports injury. The client is extremely anxious and having difficulty sleeping. Which of the following is the priority intervention?
A. Provide dim lighting in the client’s room.
B. Allow the client’s family to spend the night with him.
C. Offer music as a distraction.
D. Ask the client to tell you what he knows about the procedure.
RATIONALES
A. Providing dim lighting in the client’s room can promote sleep for some clients; however, this is not the first action the nurse should take.
B. Allowing the client’s family to stay with him can help reduce his anxiety; however, this is not the first action the nurse should take.
C. Offering music as a distraction can help reduce his anxiety; however, this is not the first action the nurse should take.
D. The first action the nurse should take is to assess the client. By determining the client’s understanding of the procedure, the nurse can provide information needed to help decrease the client’s anxiety.
LEAST RESTRICTIVE / LEAST INVASIVE: OPTION 5 FOR TEACHING CLINICAL JUDGMENT
 This framework sets priorities based on the interventions that are the least restrictive or invasive to the client to minimize the risk for harm to the client.
This framework sets priorities based on the interventions that are the least restrictive or invasive to the client to minimize the risk for harm to the client.
ITEM EXAMPLE
A nurse is caring for a client who gave birth vaginally 8 hours ago. The client reports feeling weak and dizzy. The nurse notes that the client’s perineal pad is soaked with blood. Which of the following actions should the nurse take next?
A. Administer oxygen at 10 L/minute via face mask.
B. Insert an indwelling urinary catheter.
C. Massage the fundus of the uterus.
D. Administer oxytocin 20 units in 1000 mL of lactated Ringers.
RATIONALES
A. Manifestations of postpartum hemorrhage include saturation of the perineal pad, as well as dizziness and weakness. The nurse may need to administer oxygen; however, the nurse should use a less-invasive intervention first.
B. Manifestations of postpartum hemorrhage include saturation of the perineal pad, as well as dizziness and weakness. The nurse may need to insert an indwelling urinary catheter; however, the nurse should use a less-invasive intervention first.
C. Manifestations of postpartum hemorrhage include saturation of the perineal pad, as well as dizziness and weakness. When providing client care, the nurse should first use the least-invasive intervention; therefore, the first action the nurse should take is to massage the client’s fundus.
D. Manifestations of postpartum hemorrhage include saturation of the perineal pad, as well as dizziness and weakness. The nurse may need to administer oxytocin; however, the nurse should use a less-invasive intervention first.
ACUTE VS. CHRONIC / UNSTABLE VS. STABLE / URGENT VS. NONURGENT: OPTION 6 FOR TEACHING CLINICAL JUDGMENT
 These 3 subframeworks establish the priority need based on the client condition and may be used when the other frameworks do not apply to the client-care situation.
These 3 subframeworks establish the priority need based on the client condition and may be used when the other frameworks do not apply to the client-care situation.
- ACUTE VS. CHRONIC
Addressing acute problems before chronic problems is important because there is a great risk posed for acute problems.
- UNSTABLE VS. STABLE
Unstable clients pose a greater threat than stable clients and need to receive care first.
- URGENT VS. NONURGENT
Urgent needs pose a greater threat to a client than a nonurgent need.
ACUTE VS. NONACUTE ITEM EXAMPLE
A nurse is receiving a hand-off report at the beginning of the shift for 4 clients. Which of the following clients should the nurse assess first?
A. A client who has macular degeneration and does not want to take his medication.
B. A client who is taking insulin and has an HbA1c of 7%.
C. A client who has Graves' disease and has exophthalmos.
D. A client who is taking digoxin and is experiencing anorexia.
RATIONALES
A. Macular degeneration is a chronic condition that responds to medication; although the nurse should assess the client to determine why he does not want to take his medication, this is not the client the nurse should assess first.
B. An HbA1C reflects a client’s blood glucose over the past three months; therefore, this is not the client the nurse should assess first.
C. Exophthalmos is an expected finding for a client who has Graves' disease; therefore, this is not the client the nurse should assess first.
D. This is the client the nurse should assess first, because anorexia is a possible indication of digoxin toxicity.
STABLE VS. UNSTABLE ITEM EXAMPLE
A nurse is reviewing laboratory data for four clients. Which of the following clients should the nurse assess first?
A. A client who has atherosclerosis with a total cholesterol level of 250 mg/dL.
B. A client who has chronic kidney disease with a BUN of 80 mg/dL.
C. A client who is receiving warfarin with an INR of 4.0.
D. A client who is receiving furosemide and has a serum potassium of 3.8 mEq/L.
RATIONALES
A. The nurse should continue to monitor the client who has atherosclerosis and an elevated total cholesterol level; however, this client is stable and does not need to be assessed first.
B. The nurse should continue to monitor the client who has chronic kidney disease and an elevated BUN; however, this client is stable and does not need to be assessed first.
C. A client who is receiving warfarin and has an INR of 4.0 is at risk for hemorrhage. The nurse should assess this client first.
D. The nurse should continue to monitor the client who is receiving furosemide and has a potassium level within the expected reference range; however, this client is stable and does not need to be assessed first.
URGENT VS. NONURGENT ITEM EXAMPLE
A nurse is caring for a client who has peripheral arterial disease. Which of the following findings should the nurse report to the provider immediately?
A. Report of intermittent claudication
B. Shiny, hairless lower extremities
C. Absent dorsalis pedis pulse
D. Dependent rubor.
RATIONALES
A. Report of intermittent claudication is an important finding; however, it is common for clients with peripheral arterial disease to have this type of pain.
B. Shiny, hairless lower extremities is an important finding; however, clients with peripheral arterial disease usually develop this from long-term impaired circulation.
C. The priority finding is an absent dorsalis pedis pulse. This can indicate acute arterial occlusion, which requires immediate intervention.
D. Dependent rubor is an important finding; however, clients with peripheral arterial vascular disease usually develop this from long-term impaired circulation.
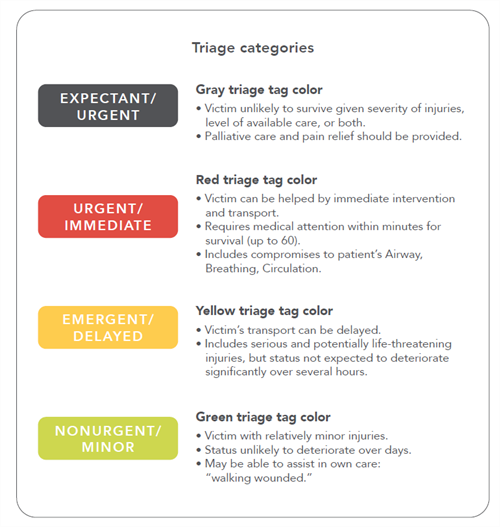
SURVIVAL POTENTIAL
This is a triage system used during mass-casualty events to determine priorities of care for all injured clients.
 Triage categories
Triage categories
EXPECTANT/URGENT
Gray triage tag color
• Victim unlikely to survive given severity of injuries, level of available care, or both.
• Palliative care and pain relief should be provided.
URGENT/IMMEDIATE
Red triage tag color
• Victim can be helped by immediate intervention and transport.
• Requires medical attention within minutes for survival (up to 60).
• Includes compromises to client’s Airway, Breathing, Circulation.
EMERGENT/DELAYED
Yellow triage tag color
• Victim’s transport can be delayed.
• Includes serious and potentially life-threatening injuries, but status not expected to deteriorate significantly over several hours.
NONURGENT/MINOR
Green triage tag color
• Victim with relatively minor injuries.
• Status unlikely to deteriorate over days.
• May be able to assist in own care: “walking wounded.”
ITEM EXAMPLE
A nurse is assessing clients at a mass-casualty event and placing the appropriate triage color tag on each client. Which of the following tags should the nurse assign to a client with an abdominal wound that has eviscerated?
A. Black, "expectant" tag
B. Red, "emergent" tag
C. Yellow, "urgent" tag
D. Green, "nonurgent" tag.
RATIONALES
A. A black expectant tag indicates the client has injuries that are not consistent with life; therefore, the nurse should not issue a black expectant tag to a client who has an abdominal wound that has eviscerated.
B. A red emergent tag indicates the client has injuries that are life-threatening and need immediate attention; therefore, the nurse should issue a red emergent tag to this client.
C. A yellow urgent tag indicates the client has injuries that need attention but are not life-threatening; therefore, the nurse should not issue a yellow urgent tag to a client who has an abdominal wound that has eviscerated.
D. A green nonurgent tag indicates the client has minor injuries that do not need immediate treatment; therefore, the nurse should not issue a green nonurgent tag to a client who has an abdominal wound that has eviscerated.
When you’re looking for more information on the NCLEX, Next Gen NCLEX, and clinical judgment, visit the NGN Resource Center. And download our new Next Generation NCLEX Guidebook, the industry’s first and only publication that is an all-encompassing reference about the NGN.

