TELEHEALTH IS THE FUTURE & NOW IS THE TIME TO TEACH ABOUT IT
THE 6 TYPES OF TELEHEALTH & THE NEW WAYS MEDICINE IS USING IT
 If you didn’t already see the value in teaching your students about telehealth, the pandemic brought it into stark focus. For many clients, since March 2020, digital technology provided the only safe option for meeting with healthcare providers. Soon after the pandemic began, in fact, the Centers for Disease Control released a paper that detailed a 154% increase in telehealth visits during the last week of March 2020 compared with the same period in 2019. More recently, an article in Healio (February 2021) said that telehealth visits accounted for about 30% of total outpatient visits early in the pandemic. And even more recent analysis indicates telehealth use has increased 38x from a preCOVID-19 baseline — a figure at which current use has now stabilized.
If you didn’t already see the value in teaching your students about telehealth, the pandemic brought it into stark focus. For many clients, since March 2020, digital technology provided the only safe option for meeting with healthcare providers. Soon after the pandemic began, in fact, the Centers for Disease Control released a paper that detailed a 154% increase in telehealth visits during the last week of March 2020 compared with the same period in 2019. More recently, an article in Healio (February 2021) said that telehealth visits accounted for about 30% of total outpatient visits early in the pandemic. And even more recent analysis indicates telehealth use has increased 38x from a preCOVID-19 baseline — a figure at which current use has now stabilized.LEARN MORE ABOUT ATI'S NEW TELEHEALTH SIMULATION.
So, if you had any previous hesitation about spending time educating students about telehealth, rest assured your efforts will not be wasted.
TELEHEALTH IS EMPHASIZED BY AACN AND QSEN
Students need to use telehealth effectively, so clients feel like they’ve gotten the most out of a visit. That means students should be practicing telehealth while they are in school to ensure they are proficient when they enter practice.
Major nursing organizations have incorporated telehealth into their guidance documents. For example, the American Association of Colleges of Nursing (AACN) includes telehealth in Section 8 of its Informatics Essentials. In this section, it advises educators to:
- Identify the basic concepts of electronic health, mobile health, and telehealth systems for enabling patient care.
- Demonstrate appropriate use of information and communication technologies.
- Deliver care using remote technologies.
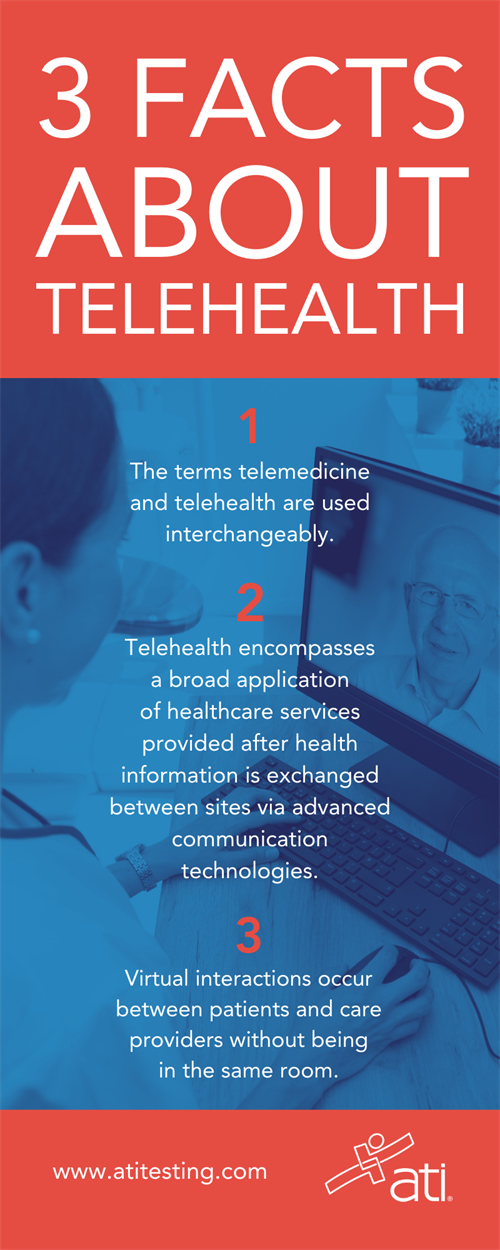
DOWNLOAD THE INFOGRAPHIC AT RIGHT AS A HANDY REFERENCE
Similarly, the Quality and Safety Education for Nurses Institute (QSEN) includes telehealth in its Informatics Competencies. The organization defines informatics as using “information and technology to communicate, manage knowledge, mitigate error, and support decision-making.” Subsequently, within those competencies, you’ll find the following sections that relate to teaching telehealth:
- Knowledge: Explain why information and technology skills are essential for safe patient care:
- Skills:
- Seek education about how information is managed in care settings before providing care.
- Apply technology and information management tools to support safe processes of care.
- Attitudes: Appreciate the necessity for all health professionals to seek lifelong, continuous learning of information technology skills.
- Skills:
- Knowledge: Contrast benefits and limitations of different communication technologies and their impact on safety and quality:
- Skills: Employ communication technologies to coordinate care for patients.
- Attitudes: Protect confidentiality of protected health information in electronic health records.
The competencies also include one additional skill related to telehealth: “Use information management tools to monitor outcomes of care processes.”
ADVICE ON TEACHING TELEHEALTH FROM TECH EXPERTS
 Earlier this year, 3 telehealth experts presented a webinar for ATI on the topic of how to incorporate telehealth into undergraduate nursing education. (You can access the webinar in ATI Academy after logging in to the ATI website.) During the session, Kelley Connor, PhD, RN, CHSE, Director of Simulation-Based Education, Boise State University, pointed out educators’ obligation to help students understand this aspect of healthcare.
Earlier this year, 3 telehealth experts presented a webinar for ATI on the topic of how to incorporate telehealth into undergraduate nursing education. (You can access the webinar in ATI Academy after logging in to the ATI website.) During the session, Kelley Connor, PhD, RN, CHSE, Director of Simulation-Based Education, Boise State University, pointed out educators’ obligation to help students understand this aspect of healthcare.
“As educators, part of our role is to be able to teach others how to use it as effectively as possible so that patients get what they need,” she explained. She warned against assuming that, because students are comfortable with technology, they’ll be able to pick up the use of telehealth with little instruction. The problem with that belief is that it overlooks other crucial communication skills students are lacking to effectively use telehealth.
“[Students] use things like TikTok,” Dr. Connor explained, “buy maybe they don’t have the skills to use it in a professional setting — to be able to really communicate and deliver care to patients.
UNDERSTANDING WHAT TELEHEALTH IS
 Another participant in ATI’s webinar was Lynda Peel, MSN, RN-BC, CCRN-E, Program Manager of Data and Process at St. Luke’s Health Systems (Boise, Idaho). She reiterated today’s reality about telehealth.
Another participant in ATI’s webinar was Lynda Peel, MSN, RN-BC, CCRN-E, Program Manager of Data and Process at St. Luke’s Health Systems (Boise, Idaho). She reiterated today’s reality about telehealth.
“Telehealth is not going away, and COVID has really brought that to the surface,” she said.
As a result, students need to be prepared for telehealth when they graduate.
“They should be learning about telehealth when they’re experiencing it in the clinical setting,” she added.
Before entering that clinical setting, however, students can practice telehealth using simulation tools, such as a new module within ATI’s Nurse’s Touch, the Communicator — “Client care through telehealth.” This resource provides opportunities for students to train with telehealth technologies to interact with clients who have chronic health conditions.
To kickstart your lessons, though, you might need a quick lesson yourself about telehealth — such as understanding when someone is referencing the technology, even if they’re not using the specific verbiage of “telehealth.”
Peel explained: “Telehealth is used interchangeably with the words telemedicine, e-health, and even m-health.”
The term telehealth refers to a broad scope of remote healthcare services using electronic and digital information and communication technologies. These virtual healthcare interactions occur between the originating site, where the patient is, and the distant site, where the provider is. Those two terms are important but can be confusing, Peel added.
“For years,” she admitted, “I had a sticky note on my camera to remind me the patient was the originating site. Because, when you’re documenting for CMS purposes, you need to know where the originating site is.”
She identified six different types of telehealth.
- Video visits. Synchronous (real time) or asynchronous.
- Remote patient monitoring (RPM). Use of a mobile device for daily monitoring of tests and physiologic data. (Sometimes known as remote patient management.)
- Surveillance. Purposeful, ongoing interpretation, synthesis, and analysis of individual patient or population data to support clinical decision-making.
- Store-and-forward. Images or videos that are sent for asynchronous review.
- eVisits. Virtual interactions (emails, patient portals, phone calls, text messages, etc.) between patients and providers.
- Mobile health. The use of smart devices (smart phones, tablets, and wireless wearable technology devices) to track activity, physiologic data, and other personal health metrics.
VIDEO VISITS: TELEHEALTH TYPE NO. 1
In explaining the six, Peel recognized that when most people think of telehealth, they think of video visits. These interactions can be in real time or asynchronous.
Some real-time visits are facilitated by a telepresenter at the originating site, while some less-complicated visits are patients only. Telepresenters can be nurses or nonlicensed personnel. This information is important to know, Peel pointed out, because — if the individual is licensed — you need to know that person’s scope of practice.
RPM: TELEHEALTH TYPE NO. 2
Peel explained that RPM uses mobile devices to capture patient data, which is asynchronously analyzed by a clinician. The clinician then makes a decision based on that data.
“A good example of RPM,” she added, “is a heart-failure program where patient weights, blood pressures, and perceived dysthymia on exertion are analyzed for acute conditions.”

Upon receiving and reviewing this information, a nurse makes clinical decisions on whether to call the patient.
“RPM has traditionally been used only for chronic conditions,” Peel explained, “but in this COVID era, it’s getting [used] more and more [for] acute conditions."
SURVEILLANCE: TELEHEALTH TYPE NO. 3
Surveillance is purposeful, ongoing data-monitoring and collection. A good example? Tele-ICU, where hundreds of patient data points are continuously analyzed to alert providers to conditions from acute to concerning trends.
Tele-ICUs also use video surveillance via 2-way audio-video to help assess patients, assist and mentor bedside clinicians, and educate patients.
Knowing a camera is in the room is important knowledge for new nurses, Peel noted, because the cameras offer a level of additional support.
“In most cases, there are people on the other side of those cameras who are there to help, who have years of experience, and who can answer questions for them or talk things through,” Peel explained.
STORE-AND-FORWARD: TELEHEALTH TYPE NO. 4
Also referred to as asynchronized telehealth, this technology involves gathering data from a client, and then sending it via a secure e-mail or messaging service to a cloud-based platform. The data is analyzed, and a diagnosis and treatment plan is sent back to the patient or provider.
Only a few years ago, store-and-forward was used almost exclusively by dermatologists and ophthalmologists. Nowadays, however, primary care programs are putting the option to use.
A good example of this technology, Peel said, is sending MRI images in the middle of the night to a site on the other side of the world where it’s daytime, “like Israel,” she explained, “because that’s where a tele-stroke program is.”
eVisit: TELEHEALTH TYPE NO. 6
The American Academy of Family Physicians defines an eVisit as an “evaluation and management service provided by a physician or other qualified health professional … using a web-based or similar electronic-based communication.”
One of the most common platforms for eVisits are online patient portals.
MOBILE HEALTH: TELEHEALTH TYPE NO. 7
“Mobile health is very popular,” Peel said. “It’s the use of smart devices to track health metrics. This allows patients to be more engaged in their health by enhancing their involvement and gathering data.
She noted that you can expect to hear a similar term, digital health, being used more frequently in the future.
“Digital health is about transforming healthcare by applying digital technologies to prevent disease and tailor medicine to individual needs,” she explained.
HOW STUDENTS MAY ENCOUNTER TELEHEALTH IN THE FIELD
As more healthcare providers begin using telehealth, the more often that opportunities will arise in which new nurses experience the technologies.
 Teresa Rincon, PhD, RN, CCRN-K, FCCM, Director of Clinical Operations and Innovation for Telehealth, University of Massachusetts Memorial Healthcare, Assistant Professor at University of Massachusetts Graduate School of Nursing (Worcester, Mass.), was the third member of the webinar panel. She described how a physician at UMass used telehealth with pulmonary sleep patients. The doctor said she believed she provided better assessments via virtual technology than in-patient visits because she could see into the client’s home.
Teresa Rincon, PhD, RN, CCRN-K, FCCM, Director of Clinical Operations and Innovation for Telehealth, University of Massachusetts Memorial Healthcare, Assistant Professor at University of Massachusetts Graduate School of Nursing (Worcester, Mass.), was the third member of the webinar panel. She described how a physician at UMass used telehealth with pulmonary sleep patients. The doctor said she believed she provided better assessments via virtual technology than in-patient visits because she could see into the client’s home.
“She could not only look in their mouths and do a physical assessment,” Dr. Rincon said, “but she could look at their equipment and how they had it set up, and where they had it set up, and where they slept, and all kinds of other things that can impact sleep.”
Palliative care is also increasingly using telehealth.
“We have a program using telehealth video visits to engage with patients for end-of-life discussions with our palliative care experts,” Dr. Rincon said. “We’re able to bring in family members from literally all over the world to participate in those discussions. It’s really important as we talk about care management, especially for those very difficult end-of-life discussions.”
Other field uses include behavioral health, where Dr. Rincon gave the example of being able to e-prescribe Suboxone to help reduce opioid cravings. Behavioral health practitioners are also using telehealth for suicide screenings.
“Just so much is happening in the areas of telehealth,” Dr. Ricon summarized. “Really, the sky’s the limit of where we can take this.” However, she added that these new opportunities made it that much more important for nurse educators to teach students about telehealth.

 Simulations are one of the most effective tools for such teaching, especially due to the limitations that clinicals present. An educator who tested ATI’s “Client care through telehealth” module (within ATI’s Nurse’s Touch, The Communicator), said the tool was helpful “because I don’t think a lot of our students will get to experience a telehealth [visit].”
Simulations are one of the most effective tools for such teaching, especially due to the limitations that clinicals present. An educator who tested ATI’s “Client care through telehealth” module (within ATI’s Nurse’s Touch, The Communicator), said the tool was helpful “because I don’t think a lot of our students will get to experience a telehealth [visit].”
Similarly, another educator who participated in a pilot of the tool said, “The way this virtual patient reacted to some of my responses was really valuable” and “realistic.”
“We don’t typically put them in these situations in clinicals,” the educator added. “Then they see it later and are taken aback.”
Some of the specifics of the new resource include lessons on:
- Motivational interviewing techniques
- Professionalism using telehealth
- Telehealth best practices.
Students then practice interacting with clients who have chronic health conditions using two simulated telehealth conversations. Additional options within the module include a student “pull-out tab” and an interactive, downloadable PDF checklist. Together, these resources help students better retain content, navigate conversations while applying learning content, and enable easy notetaking.
Resources like the new Nurse’s Touch module fit perfectly with Dr. Rincon’s advice. She emphasized that students need to learn how, as nurses, they can use telehealth tools to further their practice and provide better care for clients.
Simulated telehealth visits are an effective first step toward reaching that goal. Ensure your students are prepared for this expanding area of healthcare that is rapidly becoming the norm.