HOW TO OVERCOME YOUR FEARS OF CLINICAL REPLACEMENT
This is the guide that will help you use simulation for clinical replacement
 When the coronavirus pandemic swept the nation, colleges and universities shut down their campuses to ensure the health and safety of both students and educators. While some healthcare sites have started to allow students back into their facilities, others continue to restrict student access. As a result, many nursing programs struggle to determine how they can replace that crucial experience.
When the coronavirus pandemic swept the nation, colleges and universities shut down their campuses to ensure the health and safety of both students and educators. While some healthcare sites have started to allow students back into their facilities, others continue to restrict student access. As a result, many nursing programs struggle to determine how they can replace that crucial experience.
While a multitude of written case studies, virtual escape rooms, video scenarios, and other screen-based options are available, most require educators to develop their own lesson plans, activities, and documentation to make the learning effective and engaging. In addition, educators need to continually compare their plans against their course objectives and outcomes to make sure the clinical simulations fulfill course goals.
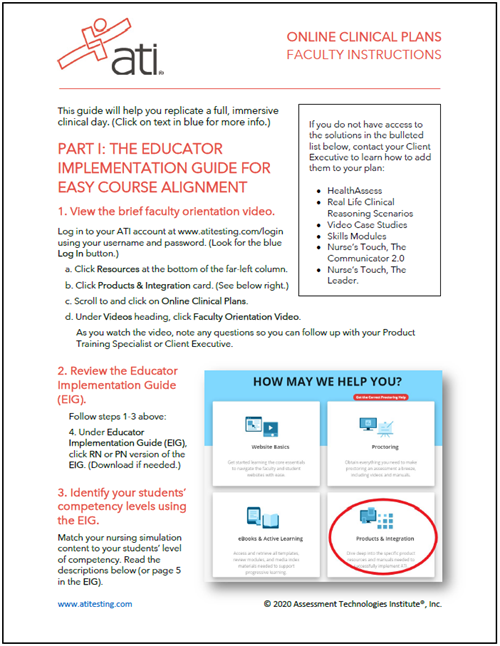
A new how-to guide, however, details how ATI’s prepared lesson plans remove the guesswork for preparing an immersive, simulated clinical-replacement day. This step-by-step manual takes educators by the hand to identify and explain the use of virtual scenarios and modules in specific ATI solutions that are part of its new Online Clinical Plans offering. (The guide also provides details on where to find the Online Clinical Plans after logging in to the Faculty Portal of the ATI website.)
If your nursing program does not currently have access to the ATI solutions explained in its Online Clinical Plans, contact your Client Executive or the ATI Customer Support Team to learn how to gain access to them:
- HealthAssess
- Real Life Clinical Reasoning Scenarios
- Video Case Studies
- Skills Modules
- Nurse’s Touch The Communicator 2.0
- Nurse’s Touch the Leader.
IDENTIFYING HOW CLINICAL REPLACEMENT USES SIMULATION
 In 2011, the National Council of State Boards of Nursing (NCSBN) proclaimed that up to 50% simulation can be effectively substituted for traditional clinical nursing experience. In the wake of the COVID-19 emergency, many states’ boards of nursing relaxed standards to allow a higher-substitution percentage.
In 2011, the National Council of State Boards of Nursing (NCSBN) proclaimed that up to 50% simulation can be effectively substituted for traditional clinical nursing experience. In the wake of the COVID-19 emergency, many states’ boards of nursing relaxed standards to allow a higher-substitution percentage.
Even so, with the stress of pivoting so suddenly to teaching 100% online, many educators struggled to stay ahead of their students in delivering lessons exclusively via remote teaching. They needed easier options for clinical replacement that appropriately challenged students the same way in-clinic experience does.
Online nursing simulation has been the much-needed solution for many.
Even so, teaching students remotely was new to many faculty. And an even greater number had never used online simulation. Thus, the nurse educator experts at ATI realized a fresh option was necessary to ease educators into this new world that combined online learning with clinical replacement.
Taking the lead, Christine L. Heid, PHD, RN, CNE, CHSE, Consulting Nurse Educator, and Pamela Osuri, MSN, RN, CNS, Director of NCLEX Services, began reviewing ATI’s screen-based simulation offerings to determine how to combine them into one offering that would solve the clinical-replacement challenge for faculty. Along with a team of other expert nurse educators, they identified the various skills and competencies taught within the scenarios, laid down a foundation using the “Standards of best practice: SimulationSM” created by the International Nursing Association for Clinical Simulation and Learning (INACSL), and created a wholly new offering: Online Clinical Plans.
 Recognizing that not all educators were familiar with online simulation offerings, Dr. Heid and Ms. Osuri devised a step-by-step guide to walk them through the process of replacing students’ lost clinical time with immersive simulations.
Recognizing that not all educators were familiar with online simulation offerings, Dr. Heid and Ms. Osuri devised a step-by-step guide to walk them through the process of replacing students’ lost clinical time with immersive simulations.
The guide explains how to use ATI’s Online Clinical Plans to replicate a full clinical day, including pre- and postconference, and is broken into 2 parts: “The educator implementation guide” for easy course alignment and “Faculty lesson plans” for streamlined execution.
The implementation section incorporates 3 phases developed by Dr. Heid several years ago that are now recognized by many simulationists as essential parts of sim-scenario development. Dr. Heid introduced the 3-phase concept at the 2017 INACSL Annual Conference and has incorporated it into sessions at subsequent conferences. Her phases create meaningful stages that incorporate the specific criteria of INACSL’s best practices’ documents and ensure none are overlooked.
The steps in the guide are particularly helpful for faculty who consider themselves novices at online learning, but even pro educators will find them helpful in offering quick guideposts and reminders. And, for faculty who have rarely used screen-based nursing simulations — or have never even logged on to the ATI website where they can gain access to these options — the guide includes details to lead you where you need to go.
Download the step-by-step guide for handy access when you are ready to begin using ATI’s Online Clinical Plans.
REFERENCES/RECOMMENDED READING
Center for Medical Simulation. The Basic Assumption. Available at: https://harvardmedsim.org/resources/the-basic-assumption/
Fanning, R. & Gaba, D. (2007). The role of debriefing in simulation-based learning. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare. (2):115-125.
Foronda, C.L., Fernandez-Burgos, M., Nadeau, C., Kelley, C.N., & Henry, M.N. (2020, February). Virtual simulation in nursing education: A systematic review spanning 1996-2018. Simulation in Healthcare, 15(1), p 46-54.
Gordon, R. M. (2017). Debriefing virtual simulation using an online conferencing platform: Lessons learned. Clinical Simulation in Nursing, 13(12), 668–674. https://doi.org/10.1016/j.ecns.2017.08.003.
Hayden, J. K., Smiley, R. A., Alexander, M., Kardong-Edgren, S., Jeffries, P. R. (2014). The NCSBN national simulation study: A longitudinal, randomized, controlled study replacing clinical hours with simulation in prelicensure nursing education. Journal of Nursing Regulation, 5(2, Suppl.), S3-S40. doi:10.1016/j.ecns.2010.02.00.
INACSL Standards Committee (2016, December). INACSL standards of best practice: SimulationSM: Simulation design. Clinical Simulation in Nursing, 12(S), S5-S12. http://dx.doi.org/10.1016/j.ecns.2016.09.005.
INACSL Standards Committee (2016, December). INACSL standards of best practice: SimulationSM Debriefing. Clinical Simulation in Nursing, 12(S), S21-S25. http://dx.doi.org/10.1016/j.ecns.2016.09.008.
Oriot, D. & Alinier, G. (2018). Pocket book for simulation debriefing in healthcare. Springer: Cham, Switzerland.
Rudolph, J.W., Raemer, D.B., & Simon, R. (2014). Establishing a safe container for learning in simulation: The role of the presimulation briefing. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare, 9(6), 339- 349. doi: 10.1097/SIH.0000000000000047.
Sullivan, N., Swoboda, S. M., Breymier, T., Lucas, L., Sarasnick, J., Rutherford-Hemming, T., Budhathoki, C., & Kardong-Edgren, S. (S.) (2019, May). Emerging evidence toward a 2:1 clinical to simulation ratio: A study comparing the traditional clinical and simulation settings. Clinical Simulation in Nursing, 30(C), 34-41. https://doi.org/10.1016/j.ecns.2019.03.003
